ENT Specialist Guide on Sinus Surgery in Singapore
Sinus surgery is often misunderstood as a quick fix for nasal congestion or sinus pressure. In clinical practice, it is a carefully considered medical decision made only after a thorough assessment and appropriate non-surgical treatment.
From an ENT perspective, surgery is not about taking drastic measures. It is about addressing a physical blockage or disease process when conservative treatment no longer provides adequate relief and symptoms continue to affect daily life.
Understanding the Purpose of Sinus Surgery
What sinus surgery is designed to achieve
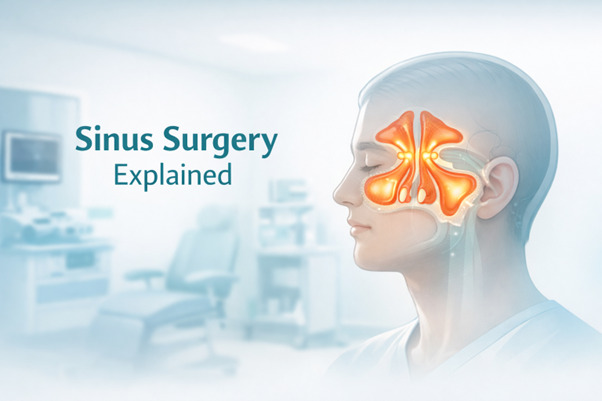
The sinuses are air-filled cavities that rely on narrow drainage pathways to remain healthy. These pathways allow air to circulate and mucus to drain naturally into the nasal cavity.
When drainage pathways become blocked, mucus accumulates and creates an environment where inflammation and infection can persist. Over time, this can lead to chronic symptoms rather than short-term illness.
Sinus surgery is designed to restore these natural drainage pathways. By improving airflow and mucus clearance, surgery reduces the conditions that allow chronic inflammation to continue, supporting long-term symptom control rather than temporary relief.
Why surgery is not the first line of treatment
Most sinus conditions improve with medical management. This may include saline nasal irrigation, nasal sprays, antibiotics when appropriate, and allergy control.
Surgery is considered only when these measures fail to provide lasting improvement. This stepwise approach ensures that patients are not exposed to unnecessary procedures.
What an ENT Specialist Is Trying to Fix

Blocked sinus drainage pathways
At the core of most surgical decisions is impaired sinus drainage. Swollen lining, narrow anatomy, or physical obstruction can prevent mucus from clearing properly.
When drainage remains compromised, symptoms such as facial pressure, nasal blockage, post-nasal drip, and repeated infections often persist.
Common underlying contributors
An ENT specialist looks beyond symptoms alone. Chronic sinusitis, nasal polyps, and long-standing inflammation are common contributors to blockage.
In some individuals, naturally narrow sinus openings or structural variations increase the likelihood of recurrent problems. Identifying these factors is essential before surgery is considered.
How ENT Specialists Decide Whether Surgery Is Appropriate
Clinical assessment and symptom history
The decision-making process begins with a detailed clinical assessment. Your ENT specialist will review symptom duration, severity, triggers, and previous treatments.
This helps distinguish temporary sinus problems from chronic disease that may benefit from surgical intervention.
Nasal endoscopy for direct visualisation
Nasal endoscopy allows the ENT to examine the nasal cavity and sinus drainage areas directly. It provides valuable information about swelling, polyps, mucus build-up, and structural narrowing.
This examination helps confirm whether physical findings align with reported symptoms.
Imaging to support surgical planning
CT imaging is commonly used to evaluate sinus anatomy and the extent of disease. It shows which sinuses are affected and how drainage pathways are blocked.
Imaging is typically reserved for cases where surgery is being actively considered.
Confirming medical treatment has been optimised
Before surgery is recommended, appropriate non-surgical treatments must be fully explored. These may include nasal irrigation, anti-inflammatory sprays, antibiotics when indicated, and allergy management.
Persistent symptoms despite comprehensive treatment may indicate the need for surgical support.
Clear Indicators That Sinus Surgery May Be Recommended

Ongoing symptoms affecting daily life
Chronic nasal congestion, facial pressure, headaches, post-nasal drip, and repeated sinus infections are common indicators that warrant further evaluation. Sleep disruption, reduced concentration, and fatigue are also frequently reported.
When symptoms persist for several months despite appropriate treatment, they can significantly affect work performance, social activities, and overall well-being. At this stage, quality of life becomes a key consideration.
ENT specialists carefully assess symptom impact alongside clinical findings. Surgery is discussed only when symptoms are persistent, meaningful, and supported by objective evidence.
Objective findings supporting surgery
Surgical recommendations are based on both symptoms and objective evidence. Endoscopy and imaging must demonstrate consistent signs of obstruction or disease.
This ensures that surgery targets a clearly defined problem.
Anatomy that promotes repeated blockage
Some patients have sinus anatomy that predisposes them to repeated blockage. Even with medication, drainage pathways may narrow again over time.
In such cases, surgery may provide more durable symptom control.
Types of Sinus Surgery an ENT Specialist May Recommend
Functional Endoscopic Sinus Surgery (FESS)
Functional Endoscopic Sinus Surgery is the most commonly performed sinus procedure. It is carried out using a thin endoscope inserted through the nostrils, allowing precise visualisation without external incisions.
During the procedure, the ENT specialist widens natural sinus openings and removes targeted obstructive tissue, such as inflamed lining or polyps. This improves ventilation and supports normal mucus drainage.
FESS is particularly useful for chronic sinusitis and more extensive disease. It is tailored to the individual’s anatomy and disease pattern rather than being a one-size-fits-all operation.
Balloon sinuplasty
Balloon sinuplasty uses a small balloon catheter to widen sinus openings gently. No tissue is removed during the procedure.
This approach may be suitable for selected patients with limited sinus disease, but it is not appropriate for all conditions.
Caldwell–Luc procedure in selected cases
The Caldwell–Luc procedure is a more traditional surgical approach used in specific situations. It creates an alternative drainage route for the maxillary sinus.
Due to its invasive nature, it is reserved for carefully selected cases.
Additional nasal procedures are performed alongside sinus surgery
Sinus surgery may be combined with procedures that improve nasal airflow. These include turbinate reduction or septoplasty when structural issues contribute to obstruction.
Addressing all contributing factors helps optimise surgical outcomes.
What to Expect on the Day of Surgery
Anaesthesia considerations
Sinus surgery may be performed under general or local anaesthesia, depending on the procedure and patient factors. General anaesthesia is more common for extensive surgery, while selected cases may be suitable for local anaesthesia.
Your ENT specialist will explain the safest and most comfortable option based on your medical history and treatment plan.
How endoscopic sinus surgery is performed
Using an endoscope, the ENT carefully identifies blocked sinus openings and areas of inflammation. Specialised instruments are used to widen drainage pathways while preserving as much normal tissue as possible.
The procedure is performed entirely through the nose. Temporary nasal packing or dissolvable materials may be placed to support healing and control bleeding.
How balloon sinuplasty is performed
For balloon sinuplasty, a small catheter is guided into the affected sinus opening. The balloon is gently inflated to widen the passage without removing tissue.
Once the pathway is opened, the balloon is removed. This allows the sinus to drain more effectively and improves airflow over time.
Expected Benefits and Realistic Outcomes
What surgery can improve
The main benefit of sinus surgery is improved sinus drainage and ventilation. Many patients report fewer infections, reduced facial pressure, and improved nasal breathing.
Better airflow often leads to improved sleep quality, reduced reliance on repeated antibiotics, and better day-to-day comfort.
What surgery does not guarantee
Sinus surgery does not eliminate the underlying tendency toward inflammation, especially in patients with allergies or chronic conditions. Medical management may still be required after surgery.
ENT specialists emphasise that surgery is part of a long-term management plan rather than a permanent cure. Realistic expectations are essential for patient satisfaction.
Risks and Safety Considerations
Common and uncommon risks
Bleeding is the most common surgical risk and is usually mild. Temporary congestion and nasal crusting are common during the healing process.
Rare complications include infection, fluid leakage near the brain, or eye-related issues. These risks are uncommon but discussed openly before surgery.
Why personalised risk assessment matters
Every patient’s anatomy is unique. Imaging and examination allow the ENT to plan surgery carefully and minimise potential risks.
Individualised planning is central to safe outcomes.
Recovery and Aftercare
Early recovery phase
Most patients experience mild to moderate discomfort for about one week. Nasal congestion, blood-stained discharge, and a feeling of pressure are common during early healing.
These symptoms usually improve gradually. Pain is typically manageable with prescribed medication.
Post-operative care priorities
Nasal irrigation is often recommended to clear debris and promote healing. Medications may be prescribed to reduce inflammation and prevent infection.
Follow-up visits allow the ENT specialist to assess healing, remove crusting, and adjust treatment as needed. Consistent aftercare plays a major role in long-term success.
When to seek medical advice
Persistent fever, increasing pain, heavy bleeding, or visual changes should be reported promptly. Early medical review helps identify and manage complications effectively.
Making an Informed Decision About Sinus Surgery
Questions worth discussing with your ENT
Have endoscopy and imaging confirmed the cause of your symptoms? Has appropriate medical treatment been fully explored?
Which surgical option best suits your condition and anatomy, and what outcomes can realistically be expected?
Final Thoughts
Sinus surgery is never recommended lightly. It is considered only when symptoms persist despite appropriate medical treatment and objective findings support intervention.
When carefully selected and expertly performed, sinus surgery can provide meaningful, long-term symptom relief. Ongoing care, realistic expectations, and open communication with your ENT specialist remain essential for the best outcome.
Frequently Asked Questions
Is sinus surgery always performed through the nose?
Most modern sinus surgeries are endoscopic and carried out through the nostrils. External incisions are rarely required.
What is the difference between FESS and balloon sinuplasty?
FESS involves removing obstructive tissue to open sinus drainage pathways. Balloon sinuplasty widens openings without tissue removal.
Why is imaging needed before surgery?
Imaging provides a detailed view of sinus anatomy and disease extent. It supports accurate and safe surgical planning.
How long does recovery usually take?
Initial recovery typically takes one to two weeks. Complete healing continues over several weeks.
When should I contact my ENT after surgery?
You should seek review if bleeding, pain, or fever worsen unexpectedly.





